Pregnancy is a crucial period for fetal development, and expectant mothers often take great care to ensure the health and well-being of their unborn children. While the dangers of traditional smoking during pregnancy are well-known, the rise of e-cigarettes (e-cigs) has led many to believe that vaping is a safer alternative. However, new research suggests that this perception may be misguided, as vaping during pregnancy can expose newborns to nicotine, toxic aerosols, and oxidative stress, potentially putting them at risk for lifelong lung issues.
In this article, we'll explore the findings of a recent review published in the journal Antioxidants, which sheds light on the impact of e-cigs on fetal and neonatal lung development. We'll delve into the stages of lung development, the role of oxidative stress and inflammation, and the long-term consequences of prenatal e-cig exposure on respiratory health. By the end, you'll have a clearer understanding of why vaping during pregnancy is not as harmless as many believe and what steps can be taken to protect the health of both mother and child.
The Stages of Lung Development and Vulnerability to E-Cig Exposure
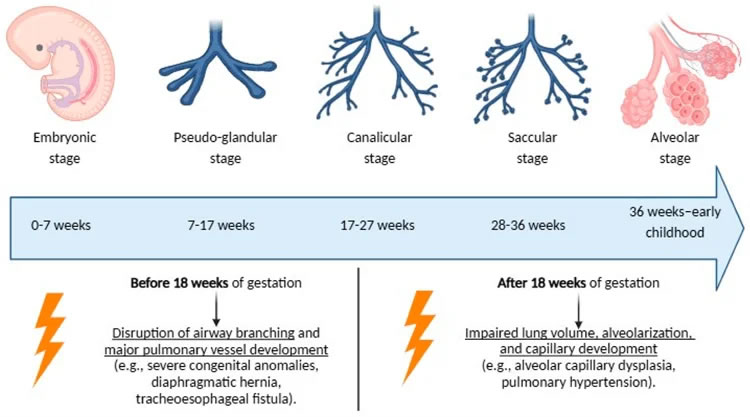
To grasp the potential impact of e-cig exposure on newborn lung health, it's essential to understand the intricate process of fetal lung development. This process occurs in five key stages:
- Embryonic
- Pseudoglandular
- Canalicular
- Saccular
- Alveolar
Each of these stages involves complex cellular differentiation and structural organization, which are necessary for proper lung function after birth. Think of it like building a house: you start with a foundation (embryonic stage), then add the walls and roof (pseudoglandular stage), install the plumbing and electrical systems (canalicular stage), and finally, furnish and decorate the interior (saccular and alveolar stages). If any of these stages are disrupted, the final product—in this case, the lungs—may not function as intended.
Environmental exposures, such as maternal smoking and air pollutants, can impair this delicate process, leading to reduced lung capacity, abnormal airway structure, and increased susceptibility to respiratory illnesses. E-cig exposure is particularly concerning because it introduces toxicants at critical developmental stages. For example, nicotine readily crosses the placenta and accumulates in fetal lung tissue, altering normal cell signaling pathways essential for airway formation. In fact, animal studies have shown that nicotine concentrations in fetal blood can be eight times higher with certain e-cig devices (e.g., JUUL) compared to traditional cigarettes.
Moreover, the solvents and flavoring agents found in e-cig aerosols contribute to oxidative stress, which is a key driver of lung inflammation and dysfunction. It's like adding fuel to the fire: not only does nicotine disrupt the normal building process, but the additional chemicals in e-cigs create a hostile environment that further hinders healthy lung development.
Oxidative Stress and Inflammatory Response: The Body's Reaction to E-Cig Exposure
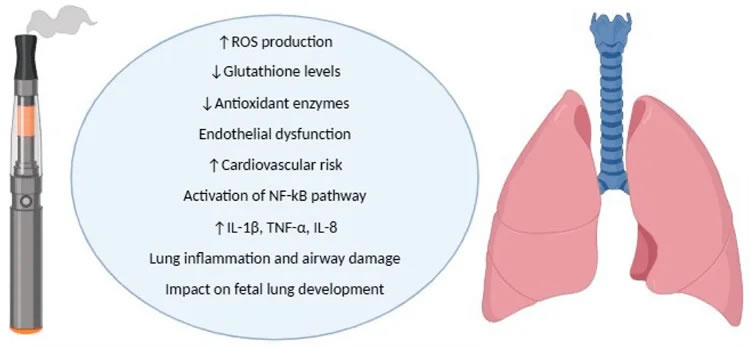
Oxidative stress occurs when the production of reactive oxygen species (ROS) exceeds the body's antioxidant defense mechanisms. You can think of it like rust on a car: just as exposure to the elements causes a car to rust and deteriorate, exposure to e-cig aerosols can cause oxidative damage to the developing lungs. This damage can lead to inflammation, impaired alveolarization (the formation of tiny air sacs in the lungs), and compromised lung elasticity in newborns.
Studies suggest that prenatal exposure to e-cig aerosols triggers an inflammatory response characterized by increased levels of interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). These pro-inflammatory markers can disrupt lung tissue remodeling, predisposing infants to respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD) later in life. It's like setting the stage for future health problems: the inflammation caused by e-cig exposure during pregnancy can have long-lasting effects on the child's respiratory health.
Furthermore, oxidative damage can interfere with pulmonary surfactant production—a process dependent on type II pneumocyte differentiation—which is crucial for lung function at birth. Pulmonary surfactant is a mixture of lipids and proteins that reduces surface tension in the lungs, allowing them to expand and contract with each breath. Without adequate surfactant, newborns may struggle to breathe effectively, leading to respiratory distress and other complications.
The Role of Nicotine, Solvents, and Flavoring Agents in Lung Dysfunction
While oxidative stress and inflammation are significant contributors to lung dysfunction, it's essential to recognize the specific roles played by nicotine, solvents, and flavoring agents in e-cig aerosols.
Nicotine exposure during pregnancy is associated with several adverse pulmonary effects. It interferes with the Notch and Wnt signaling pathways, which regulate airway branching and epithelial cell differentiation. In simpler terms, nicotine disrupts the normal "blueprint" for lung development, leading to smaller lungs, delayed alveolar maturation, and increased airway resistance in the offspring of nicotine-exposed mothers.
Moreover, nicotine affects mucociliary clearance, a critical defense mechanism against inhaled pathogens. Think of it like a conveyor belt: the cilia (tiny hair-like structures) in the lungs constantly move mucus and trapped particles up and out of the airways. Research indicates that nicotine exposure impairs ciliary function via TRPA1 receptor activation, leading to mucus accumulation and increased vulnerability to infections in newborns.
Propylene glycol (PG) and vegetable glycerin (VG), the primary solvents in e-cigarette liquids, also pose risks to developing lungs. When heated, these substances undergo thermal decomposition, releasing toxic byproducts such as formaldehyde and acetaldehyde. These substances contribute to airway irritation and damage to DNA in lung cells. In mice, maternal exposure to PG/VG reduces lung compliance (the ability of the lungs to expand and contract) in female offspring, highlighting potential sex-specific vulnerabilities.
Flavoring agents, often perceived as harmless, can also exert cytotoxic effects. Some flavors, such as cinnamon and vanilla, contain aldehydes that induce inflammation and impair normal lung cell function. Notably, multi-flavored e-cig aerosols exhibit greater toxicity compared to single-flavor variants, emphasizing the potential risks of flavored vaping products during pregnancy.
Long-Term Consequences and Prevention Strategies
The long-term consequences of prenatal e-cig exposure on respiratory health are becoming increasingly evident. Children born to mothers who used e-cigs during pregnancy have shown reduced lung function, increased rates of wheezing, and a higher likelihood of developing asthma. Additionally, e-cig exposure may suppress immune responses by impairing antimicrobial defenses like CFTR function, further exacerbating respiratory vulnerability in neonates.
To reduce the risks associated with prenatal e-cig exposure, a multi-faceted approach is necessary. Smoking cessation programs should emphasize the potential dangers of e-cigs alongside traditional tobacco products, and healthcare providers must educate expectant mothers about the risks of vaping and offer support for nicotine addiction. Legislative measures, such as restricting e-cig sales to minors and requiring warning labels on vaping products, may help reduce use among pregnant individuals.
Furthermore, antioxidant supplementation, including vitamin C, has shown promise in reducing oxidative damage. Vitamin C has been shown to prevent DNA methylation changes linked to maternal smoking, suggesting that it may help mitigate some of the harmful effects of e-cig exposure during pregnancy.
Conclusion
In conclusion, e-cigs pose significant risks to fetal and neonatal lung development due to their nicotine content, oxidative stress induction, and inflammatory effects. Nicotine disrupts key developmental pathways, while solvents and flavoring agents exacerbate airway damage. The long-term consequences include increased susceptibility to asthma, reduced lung function, and heightened vulnerability to infections.
Given the rising prevalence of e-cig use during pregnancy, urgent public health interventions are needed. Smoking cessation programs, stricter regulations, and further research into antioxidant therapies could play a crucial role in protecting infant respiratory health. Comprehensive awareness campaigns are essential to dispel misconceptions about e-cig safety and ensure that expectant mothers have the information they need to make informed decisions about their health and the health of their unborn children.
By understanding the hidden dangers of vaping during pregnancy and taking steps to reduce exposure, we can work towards a future where every child has the opportunity to develop healthy, fully functioning lungs and live a life free from respiratory disease.


